What is Filariasis? Understanding Symptoms, Transmission, and Current Treatments
Introduction
Filariasis is a debilitating parasitic disease that affects millions of people worldwide, primarily in tropical and subtropical regions. Despite being preventable and treatable, this mosquito-borne illness continues to cause significant health challenges and disabilities in endemic areas. Understanding what filariasis is, how it spreads, and the available treatment options is crucial for both prevention and management of this neglected tropical disease.
Understanding Filariasis: The Basics
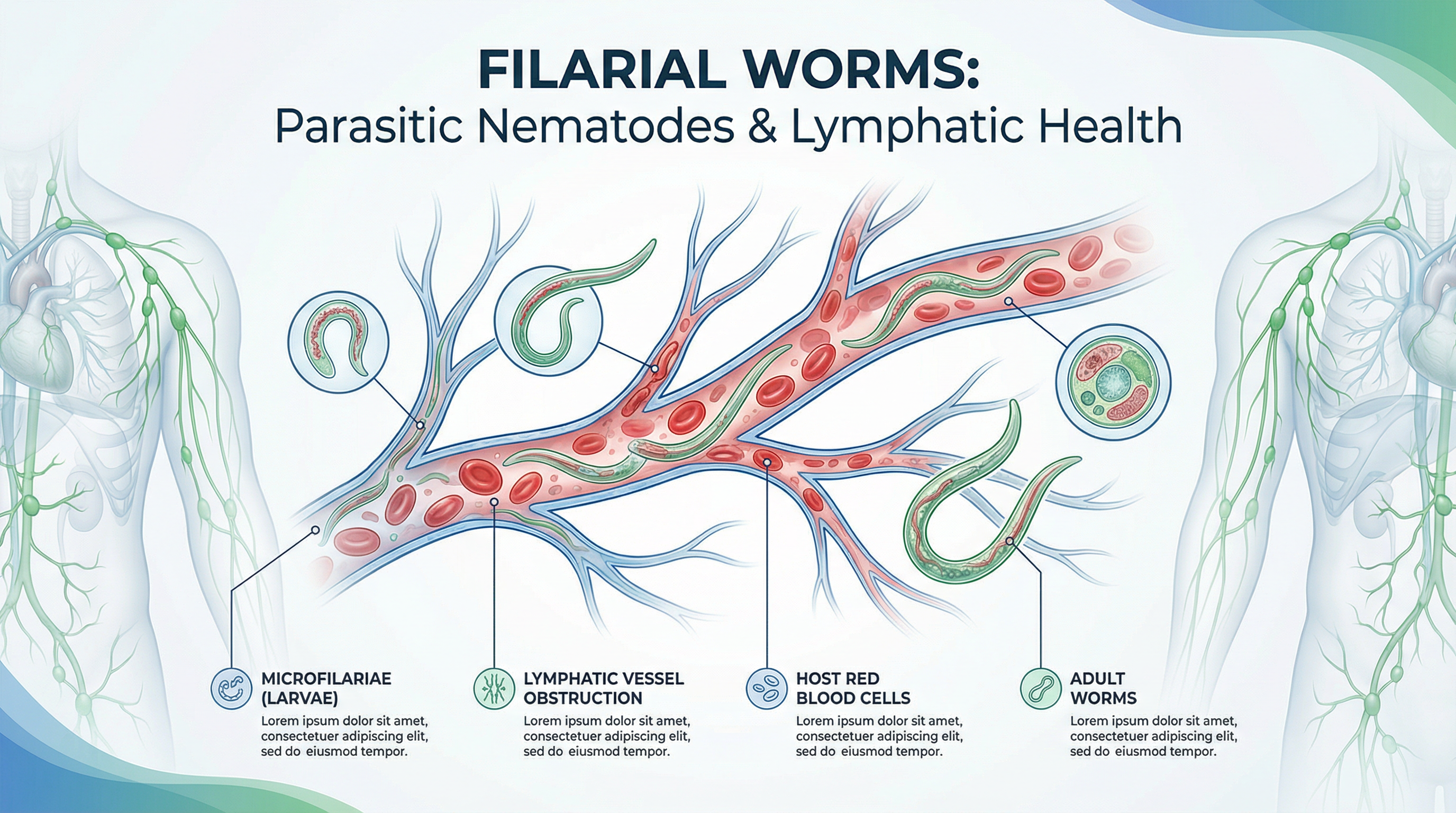
Filariasis is a parasitic infection caused by thread-like roundworms belonging to the family Filarioidea. These microscopic worms, transmitted through mosquito bites, invade the human lymphatic system, causing damage that can lead to severe swelling and disfigurement. The disease primarily manifests in three forms: lymphatic filariasis (the most common type), subcutaneous filariasis, and serous cavity filariasis.
🌡️ Concerned about unusual swelling or recurring fever? Shifam Health connects you with tropical disease specialists for accurate diagnosis!
Lymphatic filariasis, often called elephantiasis in its advanced stages, affects over 120 million people globally, with approximately 1.4 billion people living in areas where the disease is endemic. The World Health Organization has identified filariasis as one of the leading causes of permanent disability worldwide, making it a significant public health concern requiring urgent attention and action.
The disease is caused by three species of parasitic worms: Wuchereria bancrofti, responsible for 90% of cases, Brugia malayi, and Brugia timori. These parasites have complex life cycles involving both mosquito vectors and human hosts, making transmission cycles difficult to break without comprehensive intervention strategies.
The Life Cycle and Transmission of Filarial Parasites
Understanding how filariasis spreads is essential for prevention efforts. The transmission cycle begins when a mosquito carrying infective larvae bites a human. These larvae enter the body through the mosquito bite wound and migrate to the lymphatic vessels, where they mature into adult worms over six to twelve months. Adult worms can live for five to seven years in the human body.
💡 Prevention is your best defense! Let Shifam Health guide you on protective measures if traveling to endemic regions!
Once mature, female worms produce millions of microscopic larvae called microfilariae, which circulate in the bloodstream. Interestingly, microfilariae exhibit periodic behavior, typically appearing in peripheral blood during nighttime hours when mosquitoes feed most actively. This nocturnal periodicity is a remarkable evolutionary adaptation that maximizes transmission opportunities.
When another mosquito bites an infected person, it ingests these microfilariae along with blood. Inside the mosquito, the larvae develop over one to two weeks into infective forms capable of transmission. The cycle continues when this infected mosquito bites another human, depositing larvae and potentially starting a new infection. Multiple mosquito genera serve as vectors, including Culex, Anopheles, and Aedes species, depending on the geographical region.
Recognizing the Symptoms of Filariasis
Filariasis presents a wide spectrum of symptoms ranging from completely asymptomatic infections to severe, disabling manifestations. Most infections remain asymptomatic for years, with infected individuals showing no visible signs despite harboring adult worms and microfilariae. This silent period makes disease control challenging, as asymptomatic carriers continue spreading infection without realizing they’re infected.
Acute symptoms typically appear after repeated exposure to mosquito bites carrying filarial larvae. These acute episodes, called adenolymphangitis (ADL), include high fever, painful swelling of lymph nodes particularly in the groin and armpit areas, and inflammation of lymphatic vessels appearing as red, painful streaks on the skin. Patients often experience severe pain in affected areas, with episodes lasting several days before subsiding.
Acute filarial fever occurs cyclically, with attacks repeating every few months. During these episodes, patients may develop headaches, chills, and general malaise alongside localized swelling. Men may develop acute inflammation of the spermatic cord and epididymis, causing scrotal pain and swelling. These acute attacks result from the death of adult worms or immune responses to the parasites.
Chronic manifestations develop after years of infection and represent the most visible and debilitating aspects of filariasis. Lymphedema, the persistent swelling of limbs or other body parts, occurs when damaged lymphatic vessels cannot drain fluid properly. This swelling typically affects legs but can involve arms, breasts, and genitalia. Over time, affected skin becomes thickened and hardened, a condition called elephantiasis.
🏥 Don’t let symptoms progress! Shifam Health helps you access timely treatment to prevent chronic complications!
Hydrocele, the accumulation of fluid in the scrotal sac, is another common chronic manifestation affecting approximately 40 million men worldwide. This condition causes significant scrotal enlargement, often requiring surgical intervention. Some patients develop chyluria, where lymphatic fluid leaks into urine, giving it a milky appearance. This condition can lead to significant nutritional losses if untreated.
Tropical pulmonary eosinophilia is a rare but serious manifestation characterized by severe asthma-like symptoms, including coughing, wheezing, and breathing difficulties, particularly at night. This condition results from an exaggerated immune response to microfilariae trapped in lung tissues. Without treatment, it can cause permanent lung damage.
Diagnosis: Detecting Filarial Infections
Accurate diagnosis of filariasis requires specific tests performed at optimal times. The traditional diagnostic method involves examining blood samples for microfilariae under a microscope. Since microfilariae exhibit nocturnal periodicity, blood samples must typically be collected between 10 PM and 2 AM for maximum detection sensitivity. This timing requirement can make diagnosis logistically challenging.
📊 Need specialized testing? Shifam Health connects you with laboratories equipped for parasitic disease diagnosis!
Thick blood smears stained with Giemsa or other appropriate stains allow microscopists to identify and quantify microfilariae. However, this method requires trained personnel and cannot detect infections in individuals with adult worms but no circulating microfilariae. Alternative diagnostic approaches have been developed to overcome these limitations.
Immunochromatographic card tests (ICT) detect filarial antigens in blood and can be performed during daytime hours using finger-prick samples. These rapid diagnostic tests provide results within 10 minutes and don’t require electricity or specialized equipment, making them ideal for field settings. The tests detect antigens produced by adult Wuchereria bancrofti worms, offering high sensitivity and specificity.
Ultrasound imaging can visualize adult worms in dilated lymphatic vessels, a phenomenon called “filarial dance sign” where living worms create characteristic movements visible on ultrasound. This technique is particularly useful for diagnosing infections in individuals without microfilaremia. Additional diagnostic methods include antibody detection tests, PCR-based molecular diagnostics, and eosinophil counts, which are often elevated in filarial infections.
Current Treatment Options for Filariasis
Treatment strategies for filariasis focus on two main objectives: eliminating the parasites from infected individuals and managing symptoms of established disease. The primary drugs used for treating filariasis include diethylcarbamazine (DEC), albendazole, and ivermectin. These medications work by killing microfilariae and potentially affecting adult worms, though their efficacy against adult worms varies.
💊 Confused about treatment options? Shifam Health connects you with infectious disease specialists for personalized care plans!
Diethylcarbamazine remains the most widely used anti-filarial drug, effectively killing both microfilariae and adult worms. The standard treatment involves taking DEC for 12 days, though various regimens exist. Side effects can include fever, headache, and localized swelling as dying parasites trigger immune responses. These reactions are generally manageable with anti-inflammatory medications.
Combination therapy using two drugs simultaneously has become the global standard for mass drug administration programs. The WHO recommends annual single-dose treatments combining albendazole with either DEC or ivermectin, depending on whether onchocerciasis (another filarial disease) is co-endemic in the area. This approach improves efficacy while simplifying treatment delivery.
For individuals with established lymphedema, morbidity management becomes crucial. This includes rigorous hygiene practices, washing affected limbs daily with soap and water, keeping skin moisturized to prevent cracking, exercising regularly, and elevating affected limbs when resting. These simple measures can significantly reduce the frequency of acute attacks and slow disease progression.
🌟 Recovery requires comprehensive care! Shifam Health ensures you access both treatment and and post treatment followup.
Compression bandaging and specialized garments help manage lymphedema by promoting fluid drainage. Antibiotics treat secondary bacterial infections, which commonly occur in damaged lymphatic areas and trigger acute inflammatory episodes. Patients with severe lymphedema may benefit from surgical procedures including debulking surgery to remove excess tissue or lymphovenous anastomosis to create new drainage pathways.
Hydrocele can be managed surgically through procedures that remove the fluid-filled sac surrounding the testis. This surgery significantly improves quality of life for affected men. Pain management, including anti-inflammatory medications and analgesics, helps patients cope with acute inflammatory episodes and chronic discomfort.
Newer therapeutic approaches are being researched, including drugs targeting Wolbachia bacteria, which live symbiotically within filarial worms. Eliminating these bacteria appears to sterilize adult worms and eventually kill them, offering a promising treatment avenue. Doxycycline, an antibiotic that targets Wolbachia, has shown effectiveness in clinical trials and may complement existing treatments.
Prevention Strategies and Public Health Initiatives
Preventing filariasis requires multifaceted approaches targeting both mosquito vectors and human infections. Personal protection against mosquito bites forms the first line of defense. This includes using insecticide-treated bed nets, wearing long-sleeved clothing during peak mosquito activity hours, applying mosquito repellents, and installing window screens in homes.
Vector control programs reduce mosquito populations through environmental management and insecticide applications. Eliminating mosquito breeding sites by draining stagnant water, covering water storage containers, and maintaining proper waste disposal systems significantly reduces transmission risk. Indoor residual spraying and larviciding further control mosquito populations in endemic areas.
The Global Programme to Eliminate Lymphatic Filariasis (GPELF), launched by the WHO in 2000, represents the most comprehensive effort to eliminate the disease. This initiative focuses on two main strategies: mass drug administration (MDA) to interrupt transmission and morbidity management to alleviate suffering in affected individuals. MDA programs distribute anti-filarial medications to entire at-risk populations annually, aiming to reduce microfilariae levels below transmission thresholds.
Community awareness and education play crucial roles in elimination efforts. Teaching communities about transmission mechanisms, prevention methods, and treatment availability encourages participation in MDA programs and promotes protective behaviors. Health education also reduces stigma associated with the disease, encouraging affected individuals to seek care.
Surveillance systems monitor disease prevalence and track progress toward elimination goals. These systems use transmission assessment surveys to verify whether transmission has been interrupted in treated areas. Countries achieving elimination targets must maintain surveillance for several years before being certified as filariasis-free by the WHO.
Frequently Asked Questions About Filariasis
Yes, early-stage infections can be cured with proper anti-filarial treatment, though chronic damage may be irreversible.
No, filariasis cannot spread through direct human contact; it requires mosquito vectors for transmission.
Symptoms typically appear after months to years of repeated exposure to infected mosquitoes.
Yes, children in endemic areas can become infected, though severe symptoms usually develop in adulthood.
No, only about one-third of infected individuals develop chronic manifestations like elephantiasis.
Early-stage lymphedema may improve with treatment, but advanced elephantiasis is generally irreversible.
Reinfection can occur if exposure to infected mosquitoes continues in endemic areas.
The disease rarely causes death but significantly impacts quality of life and productivity.
Conclusion: A Preventable Disease Requiring Global Action
Filariasis remains a significant public health challenge affecting some of the world’s most vulnerable populations. While the disease causes considerable suffering and disability, it is both preventable and treatable with existing tools and strategies. Understanding what filariasis is, recognising its symptoms early, and knowing available treatments empowers individuals and communities to combat this disease effectively.
The global elimination initiative has made remarkable progress, with several countries achieving elimination targets. However, sustaining these gains requires continued commitment to mass drug administration programs, vector control, and morbidity management. Individual actions, including mosquito bite prevention and participation in treatment programs, contribute significantly to elimination efforts.
For those living in or traveling to endemic areas, awareness and prevention remain paramount. Early diagnosis and treatment can prevent progression to chronic, debilitating stages of the disease. With coordinated global efforts, improved access to treatment, and continued research into new therapeutic approaches, the dream of a filariasis-free world becomes increasingly achievable.
🏥💙 Your health matters! Whether you need diagnosis, treatment, or travel medicine advice for filariasis, Shifam Health connects you with expert infectious disease specialists across India.
Get personalised consultations, access to diagnostic facilities, and comprehensive treatment support. Contact Shifam Health today—because preventing tropical diseases starts with the right guidance! 🌍✨
